Have you ever wondered how scientists discover new drugs? In this blog, we explore the journey research takes from the initial questions to new drugs.
Research gives hope for the future for so many people affected by breast cancer. Our researchers are looking to find new and more effective breast cancer treatments as well as improve existing ones to make them kinder. But have you ever wondered how scientists discover new drugs? In this blog, we explore the journey research takes from the initial questions to new drugs.
Asking the right questions
Research can take years before a new effective treatment reaches patients. In 2005, Breast Cancer Now scientists discovered that blocking a protein called PARP could destroy breast and ovarian cancer cells with changes in BRCA genes. Now, a drug called olaparib that does just this is used to treat ovarian cancer and secondary triple negative breast cancer with BRCA changes.
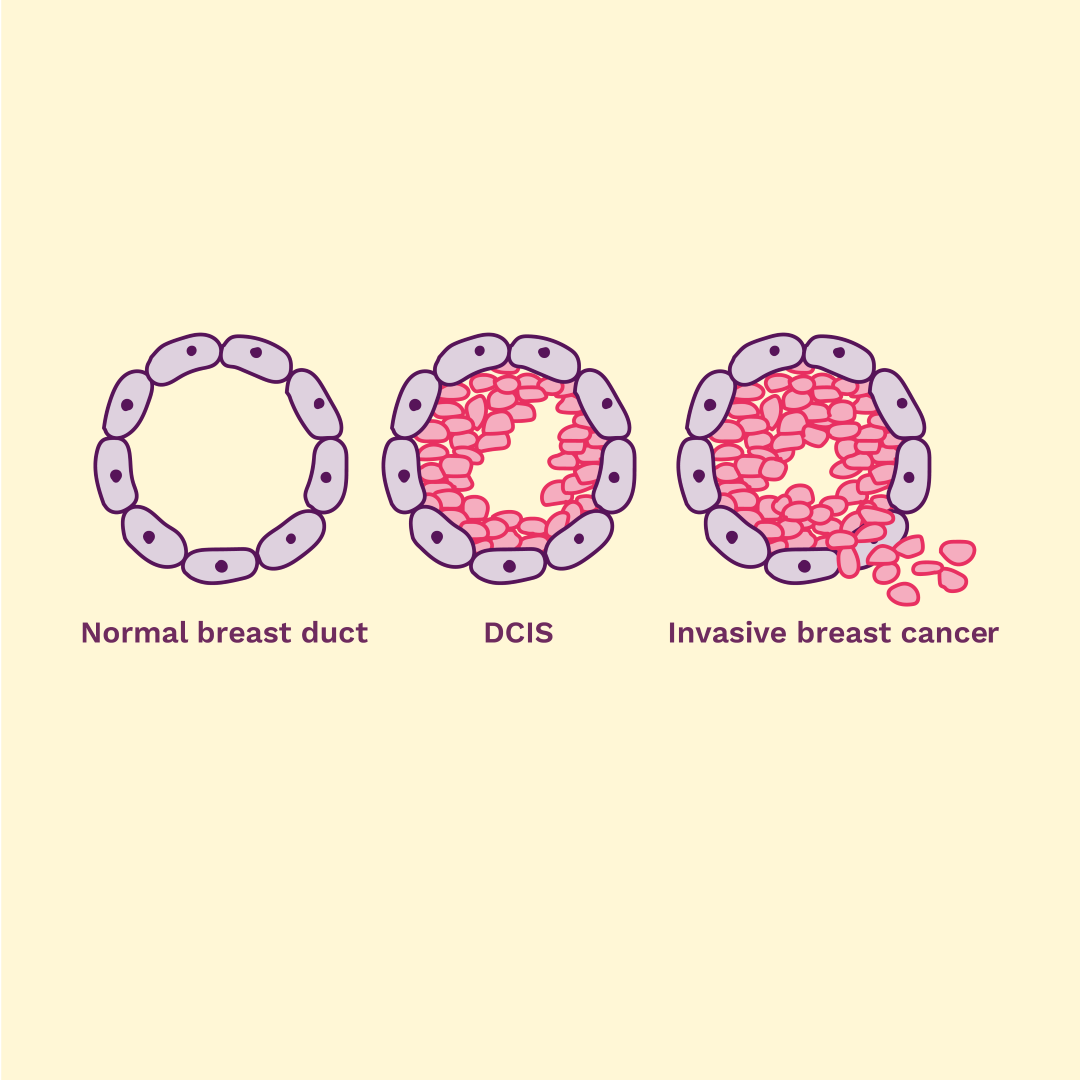
Early laboratory research is where a potential new treatment starts. When researchers look at diseases, they want to know what causes them on a molecular level. What changes mean that someone gets that disease? What roles do particular molecules play?
It is vital to understand how a disease works. Researchers need to have gone through years of education and training to be able to do that. If we understand what role a molecule or gene plays, we can find new ways to target them. It could then be used to prevent or treat the disease.
How does new knowledge reach patients?
Finding out how to use the molecular understanding of breast cancer to improve people’s lives is often called translational research. This research provides a bridge between the discoveries made in the lab and patients in the clinic.
To begin developing new drugs, scientists first need to decide what process in a cancer cell they want to target. Treatments usually target a specific molecule in cancer cells. Researchers then need to find or design a chemical compound, or a biological molecule such as an antibody. It needs to interact with the target molecule and have the desired treatment effect, turning the target on or off.
Scientists might use computer programs to carry out this design process. They could also treat cancer cells with a range of compounds to see which has the desired effect. They might need to refine their chosen drug, to make it as effective and safe as possible.
Sometimes cancer drugs work well in the laboratory, but can’t be used to treat people due to severe side effects. Researchers then need to find ways to reduce these side effects. For instance, scientists we fund are working to add a special switch to a drug called duocarmycin to make it kinder to the patient.
How does a new drug affect the whole body?
Once researchers have found a drug that works well against cancer cells, they need to see how it affects the rest of the body. This is where animal models of the disease are needed. They provide information about how well the drug reaches a tumour, whether it stops the tumour from growing, and what side effects it may have.
By law, all new drugs must first be tested on animals, but the use of animals in research is not an issue that we or our scientists take lightly. We are constantly striving to develop techniques that mean the use of fewer animals in research. We only fund animal research if it is essential and there is no alternative.
How do clinical trials work?
When laboratory research has proven that a new treatment could work, it can progress to clinical studies. But only a small proportion of drugs that enter clinical trials reach routine clinical use, as not all drugs work as well as lab experiments indicate.
Phase 1 clinical trials focus on the dosage and safety of the drug. They investigate what effect the drug has in 20 to 80 people who have run out if treatment options. Researchers watch carefully to understand the highest dose that people can have without serious side effects.
The next step is a Phase 2 trial. This involves several hundred participants who are living with the condition the drug aims to treat. They are monitored for several months or years to see how effective the drug is and what side effects it has.
Then, Phase 3 clinical trials can include up to 3,000 participants. At this point, researchers are looking to understand how the drug works when compared to existing treatments. The aim is to show that the new drug is safe and as effective. Because the study is so big, some rarer side effects can also be found. Phase 3 trials can also test whether an existing drug works better when given at a different dose or at a different point during treatment. If Phase 3 study is successful, the drug can be approved for use.
A Phase 4 clinical trial comes after a drug has been approved. It checks the drug's performance in the real world. Researchers look at long-term risks and benefits, as well as rare side effects that can only be found in large groups of people using the drug over a long time.
Why is drug development so expensive?
One of the major factors is the length of the research and development process. It can take as long as 10 years to develop new treatments.
It’s estimated that only one in 10,000 compounds will ever reach patients. Many drugs that look promising at early stages of research don’t withstand the scrutiny of further testing. The drug needs to have the desired effect on the tumour and manageable side effects. It also needs to reach cancer cells in the body. Only then it can become a successful treatment.
Developing new breast cancer drugs is a long and expensive process, but it is designed to make sure that new therapies are thoroughly checked and made as effective as possible. With your help, our scientists are getting closer to discovering how to prevent breast cancer, save lives and enable patients to live well with the disease.