Every year thousands of doctors, researchers and patient advocates descend on San Antonio in Texas for the world’s biggest breast cancer research conference. Breast Cancer Now was in attendance at this year’s San Antonio Breast Cancer Symposium from 6-10th December, joining over 7,000 delegates from more than 80 countries to be the first to hear the very latest developments in breast cancer research. Here we round up the highlights.
Aromatase inhibitors: how long is enough?
One of the very first sessions tackled a major question on the minds of patients and clinicians alike: how long should women with hormone-positive breast cancer take aromatase inhibitors for? Research in recent years has indicated that taking tamoxifen for 10 years rather than five can save lives, and that a longer duration of aromatase inhibitors prevents some breast cancers coming back, but the jury was still out on whether this could save lives too.
We heard outcomes from the DATA, IDEAL and NSABP B-42 trials, which disappointingly did not find a significant survival benefit for patients who’d taken aromatase inhibitors for longer. Professor Michael Gnant weighed up this new evidence and recommended that patients who’ve been on tamoxifen for two to five years should be offered an aromatase inhibitor for an additional 2.5 to five years. But for patients who originally took an aromatase inhibitor, he advised careful consideration: those with a higher risk of recurrence might benefit from longer treatment, but their bone health and quality of life while taking aromatase inhibitors should also be taken into account.
#SABCS16: Prof Michael Gnant's recommendations for anti-hormone therapy duration in primary breast cancer based on new trial results. #SABCS pic.twitter.com/vzOkD9xCJw
— Breast Cancer Now (@breastcancernow) December 7, 2016
Side effects in the spotlight
Recognising that quality of life can be just as important as extending lives, especially in the case of anti-hormone treatments which women take for many years, the conference gave centre stage to research tackling the side effects of treatment.
We heard results from the long-running IBIS-1 trial of nearly 4,000 women, which has been pivotal in showing that tamoxifen can prevent breast cancer in women at high risk of the disease. The study’s latest analysis looked in more depth at the concerning fact that at least a third of women in the trial had stopped taking the drug before the prescribed period of five years had ended.
Interestingly, they found that participants may have been mistaking naturally-occurring symptoms (of the menopause, for example) for side-effects of tamoxifen, and this was affecting their adherence to the drug. Dr Sam Smith concluded that women need more support to manage menopausal symptoms, whether or not they are directly caused by tamoxifen, and that this support should be given in the first 6-12 months of treatment when drop-out rates were highest. He also suggested that discussing the likelihood of experiencing natural symptoms with women might help them to distinguish these from genuine side effects. Breast Cancer Now responded to these findings, and we’re also funding vital research to help women with breast cancer get the full benefit from their tamoxifen treatment.
NEWS: Read our response to new study presented at #sabcs16 on menopausal symptoms and tamoxifen adherence. #SABCS
— Breast Cancer Now (@breastcancernow) December 9, 2016
> https://t.co/wJ5iQcBLCs pic.twitter.com/EXSCFFv4nO
Keeping cool to prevent hair-loss
Staying on the subject of side-effects, we also heard results of the first ever randomised trial of scalp cooling, which for years has been suggested as a way of reducing hair loss resulting from chemotherapy treatment. The idea is that cooling a woman’s scalp while she’s having chemotherapy reduces blood flow to the hair follicles, meaning less of the chemotherapy circulating in the blood is able to damage the follicles and result in hair falling out.
Dr Julie Nangia presented results from the Scalp Cooling Alopecia Prevention (SCALP) trial showing that scalp cooling was indeed an effective way of preventing hair loss during chemotherapy, particularly for patients taking a taxane drug. Half of the trial patients who underwent scalp cooling avoided hair-loss, whereas all of the patients who didn’t have scalp cooling lost their hair. Based on these impressive results, Dr Nangia recommended that this technology should be made available to patients. However, given that it doesn’t work for everyone, we need to see more research into the psychological impact of hair loss to help patients to cope with this distressing side effect.
The cost of progress
While many scientists at the conference spend their days in the lab finding innovative ways to outsmart cancer, doctors treating patients in the clinic know all too well that these ever smarter - yet more expensive - treatments don’t always reach the patients who need them. Dr Peter Bach is a leading expert in health policy in the US, and laid bare the worsening situation faced by healthcare systems across the world. While the US and UK healthcare systems differ greatly, his analysis of the US system sounded familiar: cancer drug prices are rising rapidly and disproportionately compared to other aspects of healthcare. With adjustment for inflation, the average monthly cost of newly approved drugs has risen 10-fold from the 1990 to today.
Another problem in the US is that some patients have to pay a certain amount of money upfront before their health insurance kicks in to cover the rest of their treatment costs, meaning many people delay the start of their treatment while they find the cash to pay their upfront bills. Dr Bach proposed a number of solutions, including value-based pricing, where the price of a drug is based on the value it brings to patients. To drive this forward he launched the Drug Abacus project in 2015, but concluded his talk by reflecting on the uncertain political time the US is entering, meaning it’s hard to know which forces will prevail.
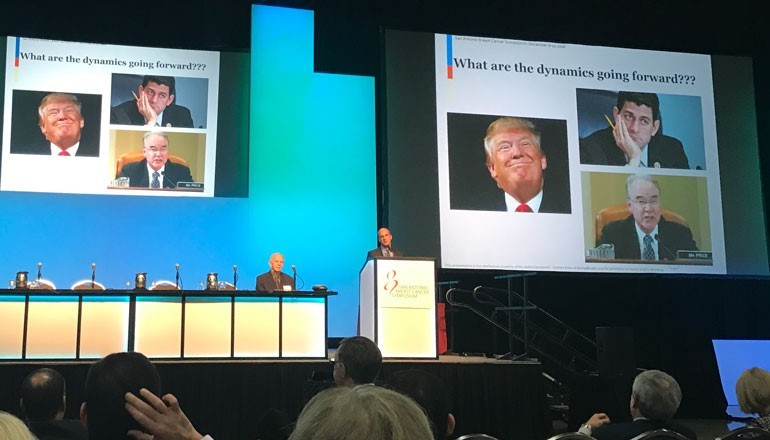
Above: Dr Peter Bach speaking on cancer drug pricing
Find out more
Read the second part of our blog covering developments in triple negative breast cancer, the BRCA genes and our hopes for 2017.