A team of scientists have recently published some research on PD-L1: a molecule found on the surface of some breast cancer cells.
PD-L1 is a molecule found on the surface of some breast cancer cells, and it helps breast tumours evade the immune system. PD-L1 does this by neutralising immune cells which might otherwise attack cancer – like sending a message that says “move along, nothing to see here”.
Drugs which stop PD-L1 doing this are currently being used as treatments for various cancers, by preventing this suppression of the immune system. The researchers behind the discovery which led to these drugs were recently awarded a Nobel Prize for their work.
However, whilst these drugs called ‘checkpoint inhibitors’ have proven to be very effective for some cancer patients, the progress in breast cancer has not been as impressive – a large number of patients who it was thought would benefit do not see any improvement in their disease.
It’s important we understand more about why this is the case, and find better ways to predict who will benefit from checkpoint inhibitors.
A closer look at ALIX
A team of scientists, led by Professor Tony Ng at the Breast Cancer Now Research Unit at King’s College London (KCL), and Dr Jeremy Carlton also from KCL, have recently published some research which could help solve this mystery.
Setting out to identify factors which make certain breast tumours more aggressive, the team found a protein called ALIX – lowering the levels of ALIX activated a survival mechanism within tumours. But exactly what ALIX does is where things get interesting.
ALIX is involved in creating tiny ball-like packages released by cells called exosomes, which for a long time were thought to be just part of the cell’s rubbish disposal system, dumping unwanted junk outside. ALIX helps sort which molecules get packed into exosomes, so the team looked at what happened when ALIX was removed from breast cancer cells. They found, to their surprise, that one molecule which was almost absent from the exosomes was PD-L1, the immune system suppressor.
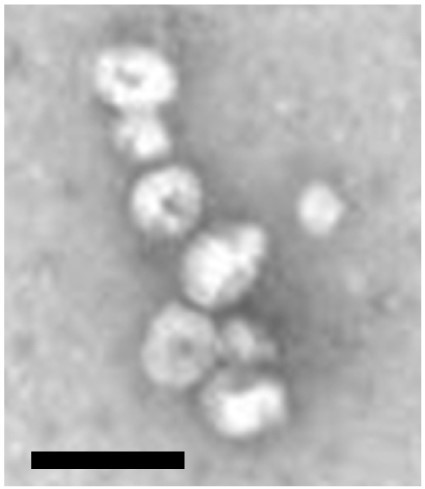
Image: a group of ball-like exosomes, observed with an electron microscope. The black bar on the image represents 100 nanometres – a length which is 100,000 times smaller than a centimetre (image adapted from Moneypenny et al (2018), Cell Reports).
Through a series of experiments using breast cancer cells in the lab, they showed that ALIX controls the balance of how much PD-L1 is on the surface of a cell and how much is packed into exosomes and sent away. Breast cancer cells which lack ALIX have lots of PD-L1 on the surface – and as a result, when implanted into mice they are more able to suppress the immune system and can grow quicker.
A checkpoint check-up
So to summarise, ALIX is helping cancer cells to survive in two ways – by activating a tumour survival mechanism, and also by stopping PD-L1 from being packaged up into exosomes, keeping it on the cell surface and blocking the immune system.
It’s still early days, but the research suggests that measuring the level of ALIX in tumours, and PD-L1 in exosomes as well as tumours, could be used to predict if a patient might benefit from checkpoint inhibitors.
What’s more, it could be relatively straightforward to analyse exosomes because they can be collected from blood. This raises the possibility of a blood test to regularly assess how patients are responding to treatment with checkpoint inhibitors.
These recent findings also shed light on the link between PD-L1 and tumour survival, which could lead to new treatment combinations for more aggressive forms of breast cancer such as triple negative.
From rubbish lorries to gold mines
Exosomes used to be thought of as little more than rubbish lorries, clearing the junk out of a cell - but opinion of exosomes is shifting thanks to research like this. Scientists are now working on the basis that they could also be an important long-distance messaging system.
For example, a team from the University of Pennsylvania, USA, studying skin cancer recently showed that the immune system can be suppressed by PD-L1 not only on the surface of the tumour, but by PD-L1 carried by exosomes – suggesting that tumours can systematically suppress the immune system around the whole body, not just in their nearby surroundings.
Conversely, there has been recent interest in using exosomes to diagnose and treat cancer. Firstly, exosomes could be used as delivery systems to package up fragile drugs inside them to make their transfer into cancer cells more efficient. And because exosomes tend to carry a selection of molecules found in the cell they originated from, researchers are also trying to use them to diagnose breast cancer and predict the aggressiveness of tumours.
No stone unturned
Sometimes researchers can be surprised by the direction their work takes them, but one thing that they are always focused on is following every potential lead to try and solve the mysteries of breast cancer. This is why Breast Cancer Now supports innovative and potentially game-changing research, to bring us closer to the day that the disease takes its last life.
The coronavirus pandemic has put a lot of our lab-based research on hold. But we don’t want to lose momentum or to let progress stall. We need your support, now more than ever, so that our researchers can make up for lost time.
Breast Cancer Now thanks the Sarah Greene Tribute Fund for their previous support towards Professor Tony Ng’s work at the Breast Cancer Now Research Unit at King’s College London.